
The Side of Rural Healthcare Not Being Talked About Enough
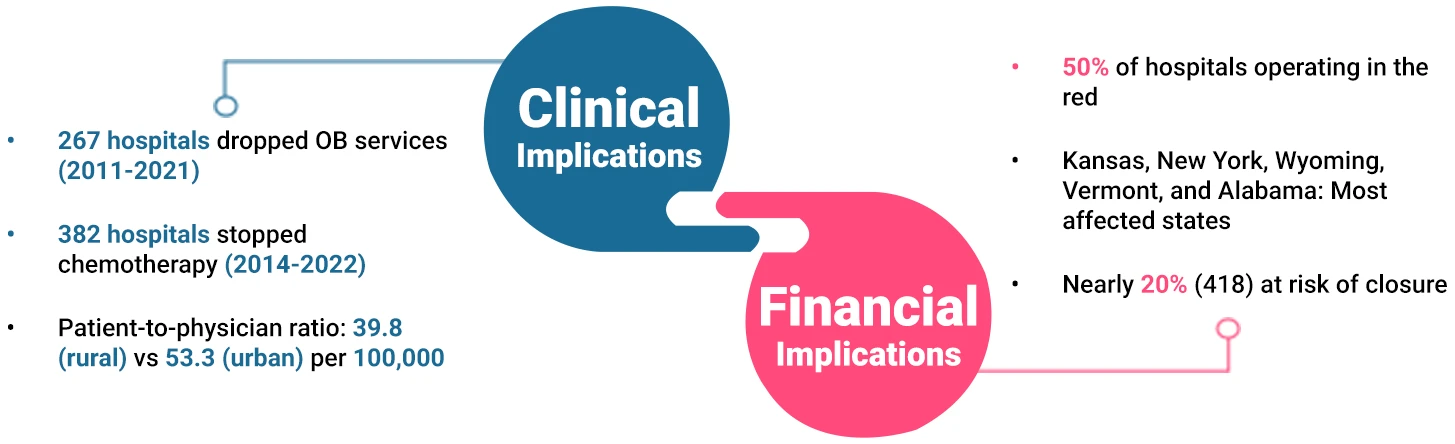
Managing rural population health with limited resources is tough already, but for many rural healthcare providers, the light has already dimmed—quite literally—with nearly 167 hospital closures since 2010.
Despite serving one-fifth of Americans, rural providers are stretching thin, and the situation will only get worse without definitive steps to restore rural healthcare.
The State of Rural Healthcare by the Numbers
Which Part of This Larger Problem Can be Solved Today?
Clinical
Financial
Statutory
Clinical
Financial
Statutory
Why RCM Leaders Need to Lead the Charge Now
Limited Patient Volume Equals Limited Topline Potential
Uncompensated Care Puts a Financial Strain
Expenses Push Operations to the Brink
Smaller population translates into fewer patients, making every dollar count but hard to realize
Fewer patients result in higher per-patient costs and limited ability to pay for care, leading to cash flow disruptions
With many uninsured / underinsured or reliant on Medicare and Medicaid, care often goes unpaid or undercompensated
This adds to the charity care cost burden on rural healthcare providers
Disproportionately high operational costs, with expenses exceeding revenue, leave rural providers in the red
Fixed costs related to staffing, essential medical equipment, and infrastructure further eats into their margins
Why RCM Leaders Need to Lead the Charge Now
Limited Patient Volume Equals Limited Topline Potential
Smaller population translates into fewer patients, making every dollar count but hard to realize
Fewer patients result in higher per-patient costs and limited ability to pay for care, leading to cash flow disruptions
Uncompensated Care Puts a Financial Strain
With many uninsured / under insured or reliant on Medicare and Medicaid, care often goes unpaid or under compensated
This adds to the charity care cost burden on rural healthcare providers
Expenses Push Operations
to the Brink
Disproportionately high operational costs, with expenses exceeding revenue, leave rural providers in the red
Fixed costs related to staffing, essential medical equipment, and infrastructure further eats into their margins
The Path Forward
Bound by geography, rural healthcare providers continue to financially bear the brunt, making revenue cycle optimization fundamental for their survival.
The dire situation demands RCM leaders to step up, take charge, and seize every opportunity to optimize costs and capture every dollar they can to maximize revenue and change the rural healthcare narrative from mere survival to sustainable growth.
By focusing on the structural framework of their RCM, they can pave the way for the sustainable financial growth of their practice. This is how:
Focusing on KPIs that Really Matter
Understanding the Root Cause Behind Revenue Leaks
Identifying the Right Levers to Pull and Push
Measuring, Adjusting, and Evolving
How Jindal Healthcare Empowers Rural Healthcare with Efficient RCM
At Jindal Healthcare, we help rural healthcare providers thrive in the volatile environment by streamlining their revenue cycle and driving their financial sustainability.
Right Expertise Driving Sustenance
Maximized Revenue, Minimized Costs
Tailored Solutions for Rural Healthcare
Our Holistic Revenue Cycle Optimization Solution Suite

- RPA bots automating 70% of the volume, freeing up rural staff for focused care
- Custom SOPs ensuring quicker auth turnaround, reducing downstream denials
- Certified coders performing accurate, compliant billing, mitigating legal risks
- AI-driven prioritization of high-value claims, maximizing reimbursements
- KPI tracking, root cause analysis, and continual feedback loop halting denials in their tracks
Our Holistic Revenue Cycle Optimization Solution Suite







