Coding Engagement
Case Study
The Client
A leading multi-specialty physician group affiliated with a nationally ranked academic health system in TX that does $5 billion in annual revenue
Scope of Engagement
The client partnered with us to manage coding validation for two high-volume service lines—Primary Care and Electrocardiogram (EKG)—with a combined monthly throughput of 40,000 claims (20,000 each). These claims were routed through Epic-based queues for validation.
Challenges Identified
- Volume-Capacity Mismatch: With high recurring claim volumes, the client faced operational strain and delays, compounded by staffing fluctuations.
- Unnecessary Workload: Overly broad validation edits triggered manual review of low-risk encounters, creating rework and congestion in Epic coding queues.
- Denial Concerns: The organization reported a 7% coding-related denial rate, impacting both cash flow and team bandwidth.
The Solution
Execution Highlights

SOP and Documentation Development
Created thorough SOPs and process documentation to standardize operations

Deployment and Scalability
Scaled to meet full monthly volumes from Day 5 onward and delivered 100% adherence to TAT from go-live

Real-Time Audits
Incorporated real-time audit checkpoints before claims were finalized

Minimize Duplication
Implemented a targeted review process to avoid duplicate validation
Provider Education
Flagged missing documentation trends for Annual Wellness Visits (AWVs) and preventive visits

Edit Optimization
Suggested claim logic to restrict AWVs to once/year to align with payer rules

Telehealth Accuracy
Recommended POS and modifier logic to reduce telehealth claim denials based on payer preferences
Emerging Impact
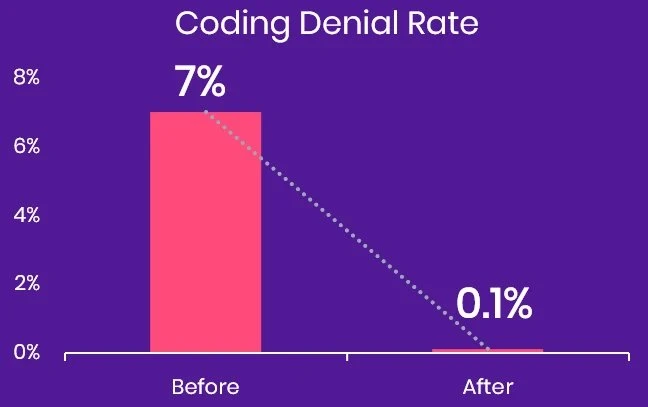
0.1%
coding denial rate on validated claims
~$4M
in additional yearly revenue gained through reduced coding denials







