The “National Hospital Flash Report: April 2023” indicates that US healthcare providers are struggling with more denials of claims. This problem influences patient treatment and happiness in addition to the financial viability of healthcare companies. Healthcare Denial Management providers have to aggressively simplify their revenue cycle handling system if they want to meet these obstacles.
Healthcare providers use this financial system for tracking, billing, and payment collecting of incoming payments. Research and Markets’ projections indicate that by 2030, the RCM market is expected to reach US$238 billion. Today, we will discuss denial management in healthcare; first, you must know the moving elements before starting denial management.
What is Denial Management in Healthcare
When a healthcare insurance payer declines to compensate a physician for services delivered to a patient based on their benefits, a claim denial results. A denial of a claim could have hundreds of different reasons.
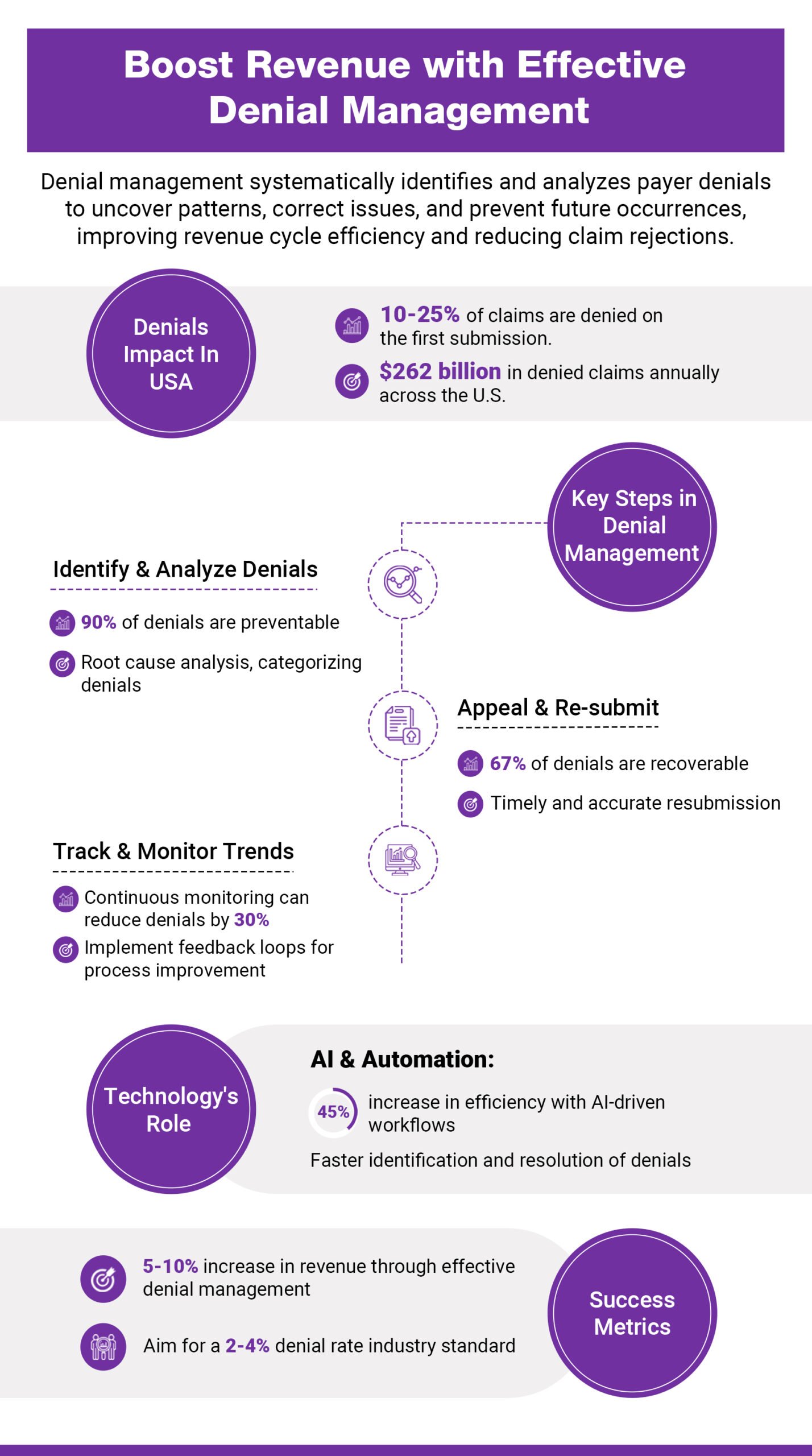
In the context of healthcare denial management is the whole process of locating, investigating, and addressing denied claims. This deliberate technique seeks to find the root of denials and set mechanisms to stop them from resurfacing. Denials of claims affect the general financial situation of the healthcare company in turn. Denials influence everything, from patient pleasure to income flow to efficiency. Strong denial management systems help to prevent denied healthcare claims that cause doctors to lose a lot of money annually.
Different Types of Denials
So, how is it conceivable that some denials are unavoidable? From a high level, there are two basic types of denials management in medical billing;
Hard Denials vs Soft Denials
Hard Denials
When a patient’s insurer flatly refuses to pay the claim, hard denials result. Usually, this occurs for insurance claims for services not covered.
Using an attractive approach won’t help when a hard denial returns to your company. Hard denials mean no income to recover from since the insurance company won’t pay you for services their customer or patient isn’t covered for. In other words, hard denials are usually written off as losses.
Soft Denials
There is a chance for recovery of income in a mild denial. Insurance evaluates a claim a patient has coverage for and rejects it due to insufficient data or lack of proof, therefore creating soft denials. Denial of soft nature is fleeting. Providers can undo their decision and get the insurance’s balance due back off.
These days, the typical inquiry that arises during every conversation is, “What type of denials do most denied claims fall under?” The solution is straightforward. Most refused claims arrive back with rejection codes falling into the soft claim bucket.
Top Reasons for Claim Denials
Becker’s Healthcare reports that, based on the frequency with which they are noted in payer denials, providers report that claimed reasons for denied claims fit the following categories:
- Prior Authorizations
- Issues with eligibility
- Inaccuracies in coding
- Incorrect modifiers
- Failure to meet submission deadlines
- Inaccuracies in patient information or claim data
Knowing these categories in great depth is crucial for assessing how to effectively create a denials prevention plan that reduces their effect on operational and financial performance.
Let’s examine every area in more depth to see how they support refuted statements.
Prior Authorization
Determining whether or not a medical service, diagnostic process, treatment plan, prescription medication, or supporting medical gadget is medically essential is known as authorization. Sometimes, the insurance company refers to this as prior authorization. It implies that the provider must verify with the payer and provide the required supporting documentation to guarantee that the element(s) in issue is acceptable and justified for the patient’s care before particular elements are given to the patient.
Eligibility Issues
Not completely grasping or knowing the patient’s coverage from the payer can lead to eligibility problems. It usually results from the provider not verifying the patient’s insurance or payment details during pre registration for the service contact. However it can also be a question of missing or erroneous patient data, like the current residence or birthdate.
Coding Inaccuracies
Among the most complex denials are those involving problems with the coded data. A certified professional coder in medical coding turns the information of a patient contact into a chargeable claim. This extensive spectrum of clinical, billing, and administrative data is set into alphanumeric codes, including CPT (Current Procedural Terminology) codes, HCPCS (Healthcare Common Procedure Coding System) codes, and the International Disease Classification (ICD) codes throughout the coding process. Most of this data is interconnected; hence, the resulting coded data can lead to many different problems.
Incorrect Modifiers
Denials based on erroneous modifiers are really a subset of the previous category, coding errors. Certain process codes use two-digit add-ons called modifiers to indicate a change in the recommended use of this procedure code.
Failure to Meet Submission Deadlines
Timely filing dates are set in the contract between the paying entity and the healthcare provider, much as previous authorizations are set. Basically, the supplier will be able to file a claim for payment following a certain service delivery for a designated term, say thirty days.
Usually, this kind of denial falls under the “hard denials” category for the straightforward reason that the deadline to submit a claim for the related care services has past, so indicating lost income.
Inaccuracies in Patient Data and Missing/Inaccurate Claim Data
This broad category covers a spectrum of possible claim problems. Regarding the patient’s coverage with the payer, it can contain erroneous, lacking, or contradicting material.
The Process of Denial Management in Medical Billing and Coding
Managing denial is a multi-stage process including claim denials’ identification, evaluation, and resolution. Reducing the number of denied claims and raising the possibility of successful appeals would help to increase the efficiency and efficacy of the income cycle.
Step 1: Identify Denials
Finding the claims that have been denied marks the first step in denial management. Reviewing remittance advice (RA) or explanation of benefits (EOB) paperwork from payers helps one identify which claims have been denied and why.
Step 2: Categorize Denials
Denials should be arranged according to the cause behind them once they have been noted. This clarifies the underlying reasons for denials for healthcare professionals so they may give their efforts to address them top priority.
Step 3: Analyze Denials
Healthcare professionals should examine the data following denials’ classification to spot trends and patterns. This study can expose typical reasons for denials and point out areas requiring process enhancement.
Step 4: Resolve Denials
Resolving rejections comes next by tackling the problems that preceded the denial. This could call for fixing coding mistakes, adding more paperwork, or resubmitting claims with the required changes.
Step 5: Prevent Future Denials
Process enhancements should ultimately be used by healthcare providers to stop denials going forward. Staff training, coding practice adjustments, or improvements to the claims submission process could all fit here.
Best Practices and Strategies for Effective Denial Management in Medical Billing and Coding
Healthcare providers should apply the following best practices in order to maximize denial management and lower the quantity of denied claims:
- Conduct Regular Staff Training: Make sure billing and coding employees are well-trained and keep current on the most recent coding rules and payer criteria.
- Implement Robust Quality Control Processes: Create robust quality control systems to examine claims before they are turned in and identify mistakes that can cause denials.
- Utilize Advanced Technology: Leverage advanced technological solutions, including automated claim scrubbing tools, to find and fix possible problems before claims are filed.
- Maintain Clear Communication with Payers: Establish good rapport with payers and have open lines of contact to promptly address problems and get an explanation of payer policies.
- Monitor Key Performance Indicators (KPIs): Track important performance indicators (KPIs). Track important performance metrics, including rejection rates and appeal success rates, to evaluate denial management initiatives and pinpoint areas that call for work.
The Importance of Denial Management in Enhancing Revenue Cycle Health
The financial situation of healthcare institutions depends critically on good denial management. Reducing denied claims can help healthcare providers boost general profitability, enhance cash flow, and lower-income loss.
Apart from the financial advantages, good denial management raises operational effectiveness and raises patient satisfaction. Quick and correct resolution of claim denials helps healthcare providers lower staff administrative load and guarantee appropriate billing for patients.
Challenges in Denial Management within Healthcare Billing and Coding
Although denial management is quite important, healthcare professionals have various difficulties putting good denial management techniques into use. These difficulties include:
- Complexity of Coding and Billing: Medical coding and billing complexity could cause mistakes and discrepancies, therefore raising the possibility of claim denials.
- Evolving Payer Requirements: Payer criteria and guidelines are always changing, which makes it challenging for medical professionals to keep current and follow all rules.
- Resource Constraints: Many healthcare institutions have limited manpower and budgets, which can impede their capacity to apply efficient denial management systems.
- Data Management Challenges: Managing and evaluating vast amounts of data can be difficult, especially for healthcare companies with limited technology capacity.
How to Improve Your Denial Management Workflow for Optimal Results
Maximizing revenue cycle performance and lowering financial losses resulting from denied claims depend on bettering denial management systems. These are various techniques to improve your process of denial management:
- Implement Real-Time Tracking and Reporting: Track and document denials in real-time using sophisticated technologies under Real-Time Tracking and Reporting. This speeds up reaction times and helps to immediately identify denial trends. Real-time data at your hands allows you to identify recurring problems and fix them before they get more serious.
- Prioritize Denials by Financial Impact: Sort denials according to financial impact; first, concentrate on those with the most financial impact. This kind of prioritizing facilitates fast recovery of major income loss. Methodically managing high-value claims will help your company’s bottom line to be much improved.
- Streamline Communication Between Departments: Make sure billing, coding, and clinical divisions have flawless communication, among other areas. Good working relationships help to lower mistakes that cause denials. Promote frequent meetings and apply integrated communication technologies to keep everyone on the same line of thinking.
- Conduct Root Cause Analysis: Frequent root cause analysis on refused claims will help you to find recurrent problems. Apply these realizations to stop future such denials. This ongoing feedback loop helps to avoid typical mistakes and improve procedures.
- Optimize Staff Training and Education: Staff should always be learning the newest coding standards, payer regulations, and denial management strategies. Well-informed employees are less prone to make mistakes, leading to denials. To keep the staff current on industry developments, think about scheduling frequent seminars and e-learning courses.
- Automate Denial Management Processes: Use automation technologies to manage regular chores, including denial tracking and claim scrubbing. Automation frees staff members to concentrate on more difficult cases and lowers hand-made mistakes. Additionally, being able to forecast possible denials before they occur can be done by investing in AI-driven solutions.
- Establish a Denial Prevention Program: Create a proactive rejection prevention program combining pre-submission reviews, eligibility verification, and documentation checks to find mistakes before claims are filed. Before claims ever get paid, our proactive strategy guarantees they are compliant and clean.
- Monitor Key Performance Indicators (KPIs): Track KPIs, including turn-around times, refusal rates, and success rates on appeals. Frequent monitoring helps to evaluate denial management initiatives’ success and points out areas needing work. Reviewing these KPIs often helps to direct strategic changes and maximize performance.
Healthcare providers can greatly boost their denial management processes by implementing these techniques, thereby improving their overall financial performance, lowering operational inefficiencies, and higher revenue recovery. These changes might significantly help your company to maintain its financial situation in a field where margins are limited, and the administrative load is great.
Discover How Texas-based Pain Management Group Improves Its Clean Payment Rate with End-to-end RCM Services
Conclusion
To sum up, revenue cycle management in healthcare depends much on denial control. Healthcare providers can streamline their rejection management systems and raise their general financial performance by knowing the typical reasons for claim denials, applying best practices, and using modern technologies.
Denial management initiatives’ success relies on a proactive strategy, ongoing development, and a dedication to lower the quantity of refused claims. Healthcare professionals can maximize their denial management processes and get better outcomes for their patients and companies by applying the guidelines described in this article.