As per the Centers for Disease Control and Prevention (CDC), 6 in 10 adults in the US have a chronic disease. Leading drivers include excessive alcohol use, lack of physical activity, and poor nutrition. While people must quickly adopt healthy new habits that last a lifetime, these statistics point towards an ever-growing demand trend for healthcare workers in the States.
Naturally, doctors, nurses and aides like laboratory technicians would run the show at healthcare facilities nationwide. That’s a fair observation, as they are the ones who treat and provide care to patients. However, many other individuals work in the background for the healthcare sector that help make visits with doctors seamless. One such function includes Revenue Cycle Management (RCM) — most pertinently, medical coding services.
What is medical coding?
Medical coding services are an integral part of Revenue Cycle Management (RCM), where an expert medical coder goes through all the clinical documentation, transcripts, and laboratory reports before applying appropriate codes. Using alphanumeric diagnoses and procedure codes, medical coders communicate critical information about patient’s medical condition and diagnosis provided (care, equipment, and medications) to the payor quickly.

Medical Coding Process
That said, the translation of diagnoses and procedures into the universal ICD-10 codes can be complex and challenging. In general, every year, medical codes are revised and updated. Many of the old codes are removed, new ones are added, and certain modifiers further specify a procedure or service. If a practitioner spends time learning medical coding and uses them for billing (basically doing the back-end analyses and paperwork), it will impact their primary objective — providing quality of care.
Did you know? Each year, claims denied due to coding errors result in the loss of about $20 billion in the US.
What is Medical Billing?
Medical billing cycle is the process of submitting and following up on claims with health insurance companies to receive payment for services provided by healthcare providers. It involves translating healthcare services into medical codes, which are then used to generate bills and claims for insurers. Medical billing is crucial for healthcare providers to receive timely and accurate reimbursement for their services. It also plays an important role in tracking patient health data and generating insights that can improve patient outcomes. Accurate medical billing ensures that healthcare providers can continue to provide quality care to patients.
Read more: Decoding the top 5 root causes for rising denials in medical billing
Why are medical coding services important in healthcare?
Without adequate ICD-10/ CPT medical coding, healthcare providers wouldn’t receive the payment for their services, which could lead to financial instability and ultimately impact patient care. Accurate medical coding also helps healthcare providers track and analyze patient health data, allowing them to identify trends and provide better care. With the healthcare industry constantly evolving, medical coding has become even more important in ensuring the delivery of high-quality and cost-effective care to patients.
Which skills are required are medical coding services?
I. Analytical Skills: Analyzing the information in the patient’s records to determine what codes are appropriate. This is an important step to ensure that the billing is foolproof and that the providers get paid in a timely manner.
II. Detail Oriented: Accuracy and attention to detail are of the highest importance to processing health insurance policies and filing bills for claims.
III. Interpersonal Skills: They need to be comfortable interacting with the other stakeholders in RCM as well as physicians and nurses. It includes everything — from discussing medical billing cycle problems, and patient information to getting other details.
Technical Skills: Most institutions use Electronic Health Records (EHR) software for all their billing and coding functions. Coding experts must be adept at these tools and understand different medical records.
Read more: Is your revenue cycle process streamlined? If not, you will continue to lose insurance money!
Conclusion:
Having a team of dedicated medical coders for your practice can be a boon as they are critical for decoding medical files and notes of doctors and assessing insurance policies before filing submissions. A high-quality medical coding team is needed for accurate and timely reimbursements as well as to ensure that the patients aren’t left paying more for a procedure than they should. This doesn’t just help the financial side of the business but also the main mission of healthcare practices, which is to provide quality, efficient and timely care for the patients. 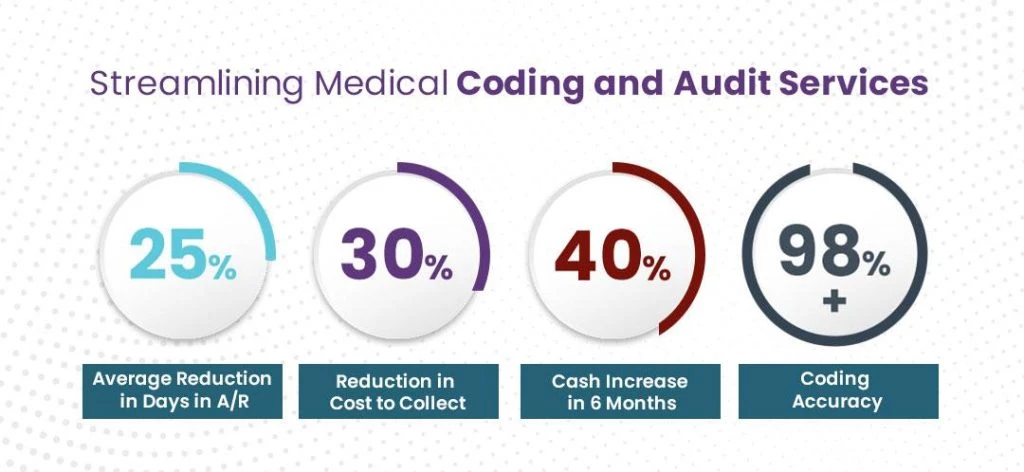
Want to know how you can strengthen your bottom line and streamline medical billing cycle by outsourcing medical billing services?