After the financial struggles many health systems faced in 2022 — with operating margins negative for 11 consecutive months according to Kaufman Hall — the revenue cycle is in the spotlight in 2023. Health system leaders are turning to their revenue cycle experts to shape their overall strategies. To navigate these challenging times and optimize financial performance, healthcare organizations are increasingly recognizing the critical role of revenue cycle management services. RCM services encompass a range of strategies, technologies, and processes aimed at maximizing revenue, improving cash flow, and enhancing operational efficiency throughout the revenue cycle.
In response to the evolving dynamics of the healthcare industry, the United States has witnessed remarkable advancements in revenue cycle management. The healthcare industry in US has witnessed different trends and advancements in revenue cycle management, including the adoption of automation technology, streamlined workflows, and improved efficiency. These trends vary across different states in the US, such as California, Texas, New York and other states, due to regional factors, demographics, policy variations, and the unique characteristics of each state’s healthcare landscape.
Certainly! Texas, as the second-largest state in the United States both in terms of population and land area, exhibits unique healthcare industry trends and challenges. Despite great progress over the last few years in RCM services in Texas, some practices still face financial challenges. There is a significant opportunity to expand access to services with new trends in healthcare revenue cycle.
Current trends in revenue cycle management services
Revenue cycle management services include the process of managing the financial aspects of healthcare, from patient registration to payment collection. The healthcare revenue cycle is a long and complex process that involves multiple steps and stakeholders. Traditionally, revenue cycle management in healthcare has been a manual and time-consuming process, with healthcare providers relying on paper-based systems and manual data entry. This has led to inefficiencies, errors, and delays in payment collection, which can have a significant impact on a healthcare provider’s financial performance.
The market is also expected to reach $100 billion by 2025, with healthcare providers increasingly looking to adopt new technologies and strategies to improve their rev cycle management.
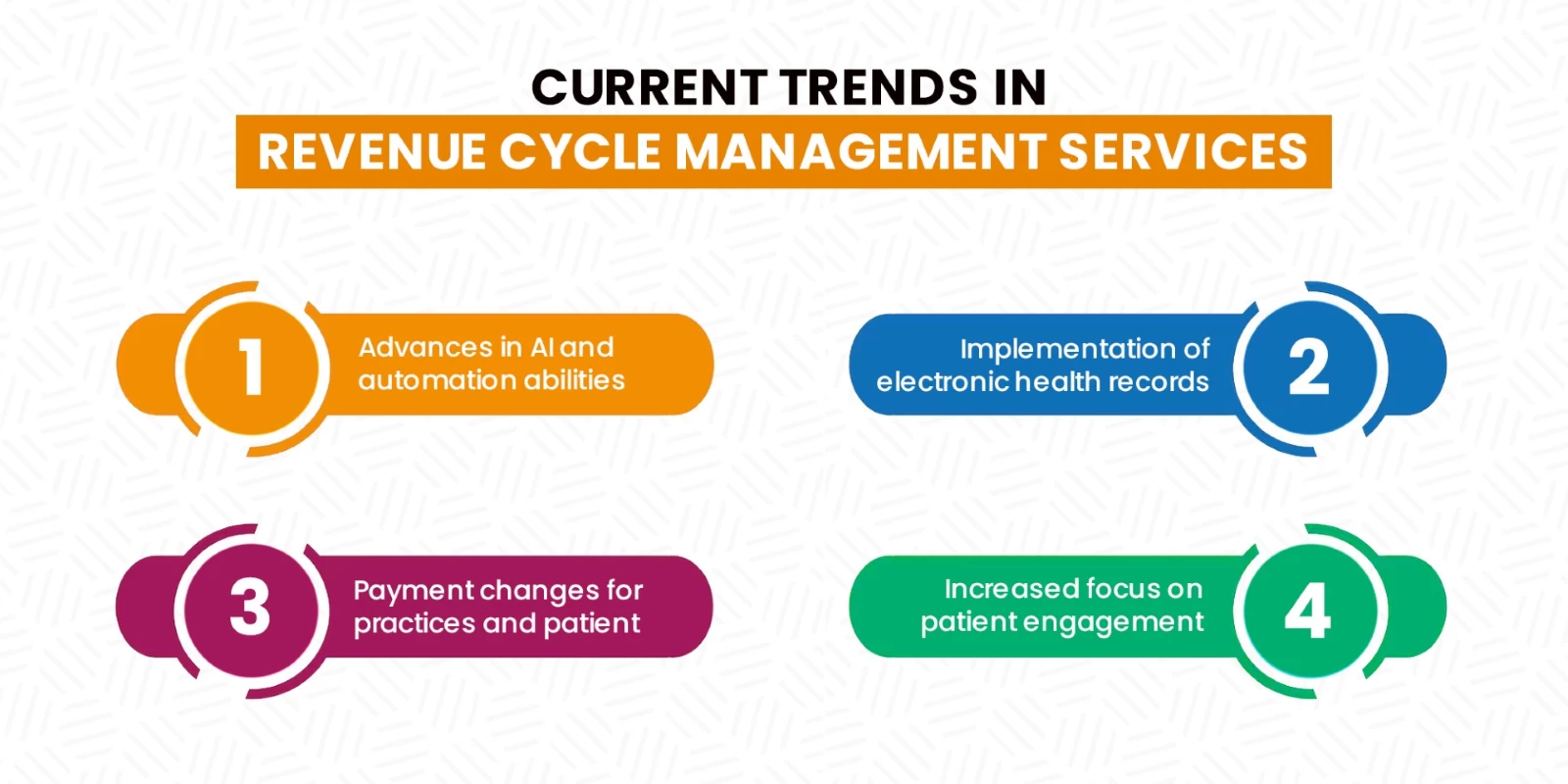
1.) Advances in AI and automation abilities
Automation in healthcare refers to the completion of repetitive tasks by a computer or robotic process. When it comes to the future of healthcare revenue cycle management services, automation is a top technology trend. Not only can it give providers and patients extra time back in their day, but it can also improve access to health data.
According to a survey, approximately 75% of health systems expressed their intention to adopt automation technology to adapt to the evolving dynamics of the RCM medical billing industry. By embracing automation in the revenue cycle, healthcare providers can expedite the process without compromising patient care quality.
Manual data entry in revenue cycle management services is prone to errors, which can result in claim denials, payment delays, and potential compliance issues. By adopting automation technology, healthcare providers can improve accuracy by eliminating human errors in data entry, claim submission, and coding processes. Automation tools can validate and verify information, ensuring completeness and accuracy before claims are submitted. This reduces the risk of claim denials, minimizes rework, and promotes clean claims submission, resulting in accelerated prior authorization, and increased revenue generation.
2.) Implementation of electronic health records
Electronic health records (EHRs) are digital versions of patient medical records that can be accessed and shared by healthcare providers. EHRs have the potential to improve revenue cycle management by streamlining the documentation and billing processes. EHRs can automate many of the manual processes involved in revenue cycle management services, such as data entry and claims processing, reducing the risk of errors and delays.
In addition, EHRs can improve patient outcomes and satisfaction by providing healthcare providers with access to real-time patient data. This can help healthcare providers to make more informed decisions about patient care, leading to better outcomes and increased patient satisfaction.
However, implementing EHRs can be a complex and costly process. Healthcare providers need to ensure that their EHR systems are integrated with their revenue cycle management processes and that staff are trained to use the new system effectively. In addition, healthcare providers need to ensure that patient data is protected and that the EHR system complies with regulatory requirements.
3.) Payment changes for practices and patient
Addressing payment changes is a significant focal point within revenue cycle management services. Payment plans, the move to credit card on file, and shift to patient as payer are all at the forefront of RCM trends. The move to credit card on file has made it easier than ever for patients, especially recurring patients, to pay faster. It gives the patient and provider more time as practices get paid faster and replace antiquated payment collection and appointment scheduling workflows.
As health care costs in the United States continue to increase, there is momentum in Texas and nationwide to achieve higher value by changing how payments take place. As per HHSC, RCM services in Texas have been designed to improve quality and outcomes for patients while reducing cost trends. These value-based approaches incentivize high-quality and cost-efficiency by linking health care payments to measures of value.
4.) Increased focus on patient engagement
Patient engagement is the process of involving patients in their own healthcare by providing them with information and resources to help manage their health. It has the potential to improve revenue cycle management by reducing the risk of denied claims and improving patient satisfaction. However, patient engagement requires healthcare providers to invest in patient education and communication tools. Healthcare providers need to ensure that patients have access to the information and resources they need to manage their health effectively. This may require investment in patient portals, educational materials, and communication tools.
The current revenue cycle management services in Texas, including the federal PHE and the DSRIP transition, informed about improved patient experience- promoting optimal health for Texans at every stage of life through prevention and by engaging individuals, families, communities, and the health care system to address root causes of poor health.
Conclusion
The healthcare industry is constantly evolving, and with it, so are the challenges facing providers. One of the most pressing challenges is managing revenue cycle management services effectively. The healthcare revenue cycle is a complex process that involves everything from patient registration and insurance verification to claims processing and payment collection. However, with the right strategies and tools, healthcare providers can streamline their revenue cycle management services and improve their financial performance.
Reference:
1.) https://www.hhs.texas.gov/reports/2022/12/texas-value-based-payment-quality-improvement-advisory-committee-recommendations-88th-texas
2.) https://www.hhs.texas.gov/sites/default/files/documents/value-based-payment-qual-improvement-recommendations-dec-2022.pdf







