The Curious Case of Telehealth: To Cover or Not to Cover?
Doctor’s appointments have taken a new form in recent years—they have gone digital!
Instead of you walking into your doctor’s office (or they ringing your doorbell for a house call), your doctor now pings your smartphone.
Yes, with telehealth, care comes to you, wherever you are, with just a click!
Telehealth is more essential than ever, driven by the changing lifestyle and the desire to overcome geographic limitations. Yet, despite its growing value, concerns around its sanctity and effectiveness are sparking debate, leading to deliberation and uncertainty around its continued coverage.
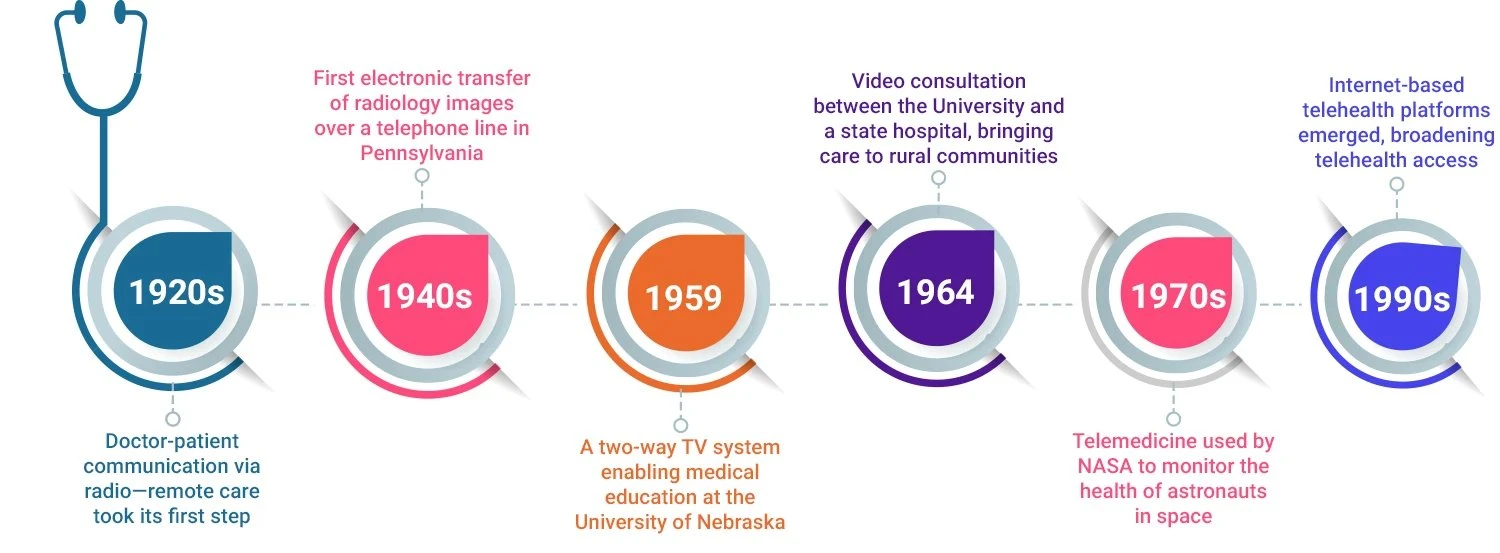
Let’s break down what’s been happening with telehealth coverage of late and how it all started.
The COVID-19 Public Health Emergency
Before the pandemic
- Patients had to reside in rural areas.
- Patients could only receive certain services via telehealth at a medical facility.
- Two-way audio-video telecommunications equipment had to be used.
Removal of Geographic and Site Restrictions
Before COVID-19, Medicare only covered telehealth for patients in rural areas, and they had to access it from approved healthcare sites (like clinics and hospitals). During the PHE, telehealth services were allowed from any geographic location (urban, rural, suburban) and could be delivered to patients at home.
Expansion of Covered Services
The list of services eligible for telehealth coverage was significantly expanded, including mental health services, physical and occupational therapy, and certain emergency department visits, making telehealth applicable across a broader range of healthcare needs.
Allowance of Audio-Only Telehealth Services
Medicare allowed audio-only (phone) consultations for patients who lacked access to video-enabled devices or the internet, ensuring that underserved populations could still receive care remotely.
Increased Provider Eligibility
More types of providers, such as therapists, clinical social workers, and speech-language pathologists, were allowed to deliver telehealth services. Previously, only certain providers, like physicians and nurse practitioners, were eligible.
Payment Parity for Telehealth and In-Person Visits
During the PHE, telehealth visits were reimbursed at the same rate as in-person visits, encouraging widespread adoption and ensuring providers weren’t financially penalized for offering virtual care.
How the Pandemic Rewrote the Telehealth Narrative
A 78-Fold Leap
Telehealth usage was 78 times higher in April 2020 than in February 2020
75% increase in telehealth encounters, from 111.4 million in 2020 to nearly 194.4 million in 2021
Why the Uncertainty?
Fraud, Misuse, and Financial Concerns
Telehealth has raised concerns about the potential for fraudulent billing and unnecessary visits, which can drive costs and create inefficiencies, prompting calls for tighter regulations and controls.
Clinical Effectiveness Limitations
Certain medical services like chronic care management may not be as effective when delivered virtually. The lack of direct interaction with patients can hinder accurate diagnoses and the quality of treatment for complex conditions.
Equity and Accessibility Barriers
Telehealth’s reliance on technology and internet connectivity can leave vulnerable populations—like those in rural areas, the elderly, or low-income individuals—disadvantaged, creating a digital divide hindering access to the same level of care as others.
Privacy, Security, and Care Gaps
Non-compliant platforms raise concerns over data privacy and security risks, while virtual care may lead to fragmented care, making it harder to coordinate treatments and maintain continuity across providers.
Provider Challenges
Telehealth may weaken the patient-provider relationship, reducing face-to-face interactions crucial for trust and effective care. Providers also face burnout due to the constant juggling of virtual and in-person visits, which may create inefficiencies in care delivery.
How Jindal Healthcare Is Leading the Charge
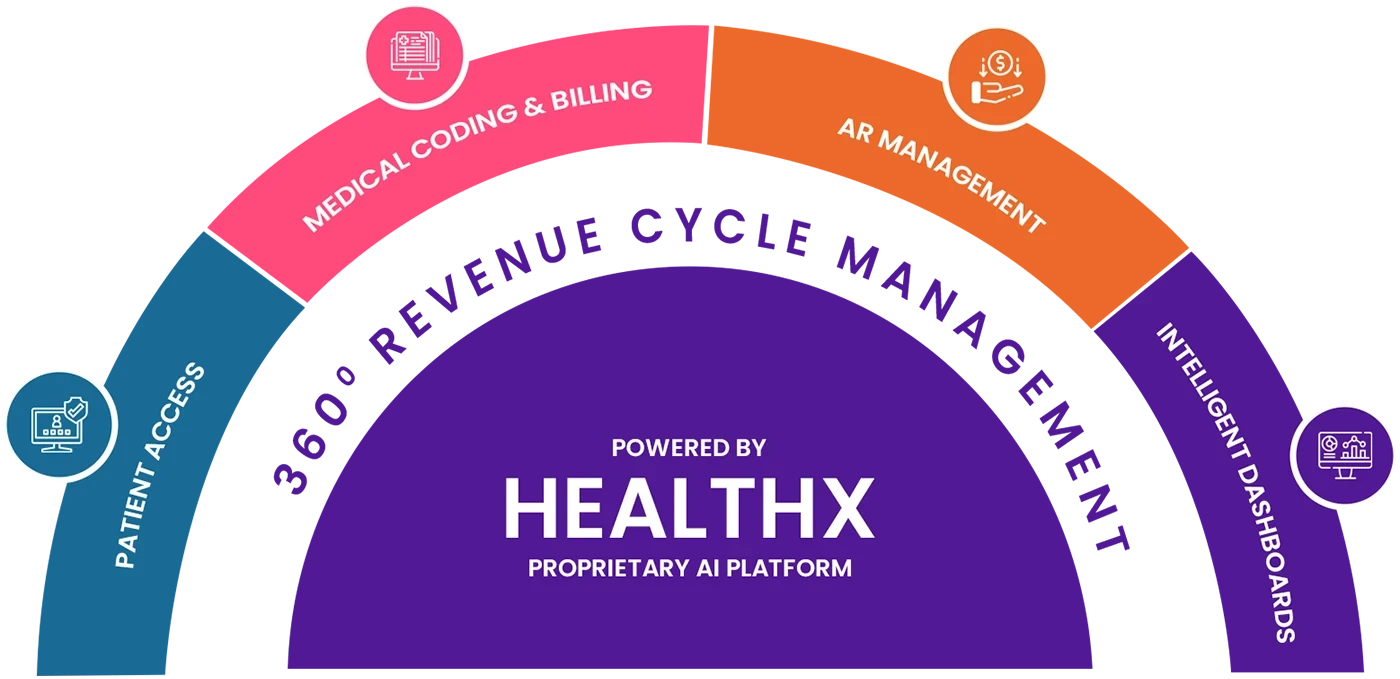
At Jindal Healthcare, we are committed to empowering healthcare providers to embrace telehealth seamlessly and effortlessly with our robust revenue cycle optimization solution suite.
Combining industry expertise with the power of the 3As of automation, artificial intelligence, and analytics, we help providers confidently navigate and realize the potential of telehealth while helping them:
Make patient access seamless with
automation-led patient verification
and SOP-guided documentation
for quick payer approvals

Navigate coding and
billing with ease with experts performing claim
scrubbing and ensuring timely
claim submissions



Navigate coding and
billing with ease with experts performing claim
scrubbing and ensuring timely
claim submissions


Transforming Healthcare with Measurable Impact
50%
Reduction in
RCM Costs
35%
Increase in
Average Revenue
60%
Reduction in 90+
Days Aging